![Healthcare_Messaging_Compliance_HIPAA_&_TCR_Integration_Guide_slide_deck_-_no_wm-1[1]](https://mytcrplus.com/wp-content/uploads/2026/01/Healthcare_Messaging_Compliance_HIPAA__TCR_Integration_Guide_slide_deck_-_no_wm-11-768x429.png)
![Healthcare_Messaging_Compliance_HIPAA_&_TCR_Integration_Guide_slide_deck_-_no_wm-2[1]](https://mytcrplus.com/wp-content/uploads/2026/01/Healthcare_Messaging_Compliance_HIPAA__TCR_Integration_Guide_slide_deck_-_no_wm-21-768x429.png)
![Healthcare_Messaging_Compliance_HIPAA_&_TCR_Integration_Guide_slide_deck_-_no_wm-3[1]](https://mytcrplus.com/wp-content/uploads/2026/01/Healthcare_Messaging_Compliance_HIPAA__TCR_Integration_Guide_slide_deck_-_no_wm-31-768x429.png)
![Healthcare_Messaging_Compliance_HIPAA_&_TCR_Integration_Guide_slide_deck_-_no_wm-4[1]](https://mytcrplus.com/wp-content/uploads/2026/01/Healthcare_Messaging_Compliance_HIPAA__TCR_Integration_Guide_slide_deck_-_no_wm-41-768x429.png)
![Healthcare_Messaging_Compliance_HIPAA_&_TCR_Integration_Guide_slide_deck_-_no_wm-5[1]](https://mytcrplus.com/wp-content/uploads/2026/01/Healthcare_Messaging_Compliance_HIPAA__TCR_Integration_Guide_slide_deck_-_no_wm-51-768x429.png)
![Healthcare_Messaging_Compliance_HIPAA_&_TCR_Integration_Guide_slide_deck_-_no_wm-6[1]](https://mytcrplus.com/wp-content/uploads/2026/01/Healthcare_Messaging_Compliance_HIPAA__TCR_Integration_Guide_slide_deck_-_no_wm-61-768x429.png)
![Healthcare_Messaging_Compliance_HIPAA_&_TCR_Integration_Guide_slide_deck_-_no_wm-7[1]](https://mytcrplus.com/wp-content/uploads/2026/01/Healthcare_Messaging_Compliance_HIPAA__TCR_Integration_Guide_slide_deck_-_no_wm-71-768x429.png)
![Healthcare_Messaging_Compliance_HIPAA_&_TCR_Integration_Guide_slide_deck_-_no_wm-8[1]](https://mytcrplus.com/wp-content/uploads/2026/01/Healthcare_Messaging_Compliance_HIPAA__TCR_Integration_Guide_slide_deck_-_no_wm-81-768x429.png)
![Healthcare_Messaging_Compliance_HIPAA_&_TCR_Integration_Guide_slide_deck_-_no_wm-9[1]](https://mytcrplus.com/wp-content/uploads/2026/01/Healthcare_Messaging_Compliance_HIPAA__TCR_Integration_Guide_slide_deck_-_no_wm-91-768x429.png)
![Healthcare_Messaging_Compliance_HIPAA_&_TCR_Integration_Guide_slide_deck_-_no_wm-10[1]](https://mytcrplus.com/wp-content/uploads/2026/01/Healthcare_Messaging_Compliance_HIPAA__TCR_Integration_Guide_slide_deck_-_no_wm-101-768x429.png)
![Healthcare_Messaging_Compliance_HIPAA_&_TCR_Integration_Guide_slide_deck_-_no_wm-11[1]](https://mytcrplus.com/wp-content/uploads/2026/01/Healthcare_Messaging_Compliance_HIPAA__TCR_Integration_Guide_slide_deck_-_no_wm-111-768x429.png)
![Healthcare_Messaging_Compliance_HIPAA_&_TCR_Integration_Guide_slide_deck_-_no_wm-12[1]](https://mytcrplus.com/wp-content/uploads/2026/01/Healthcare_Messaging_Compliance_HIPAA__TCR_Integration_Guide_slide_deck_-_no_wm-121-768x429.png)
![Healthcare_Messaging_Compliance_HIPAA_&_TCR_Integration_Guide_slide_deck_-_no_wm-13[1]](https://mytcrplus.com/wp-content/uploads/2026/01/Healthcare_Messaging_Compliance_HIPAA__TCR_Integration_Guide_slide_deck_-_no_wm-131-768x429.png)
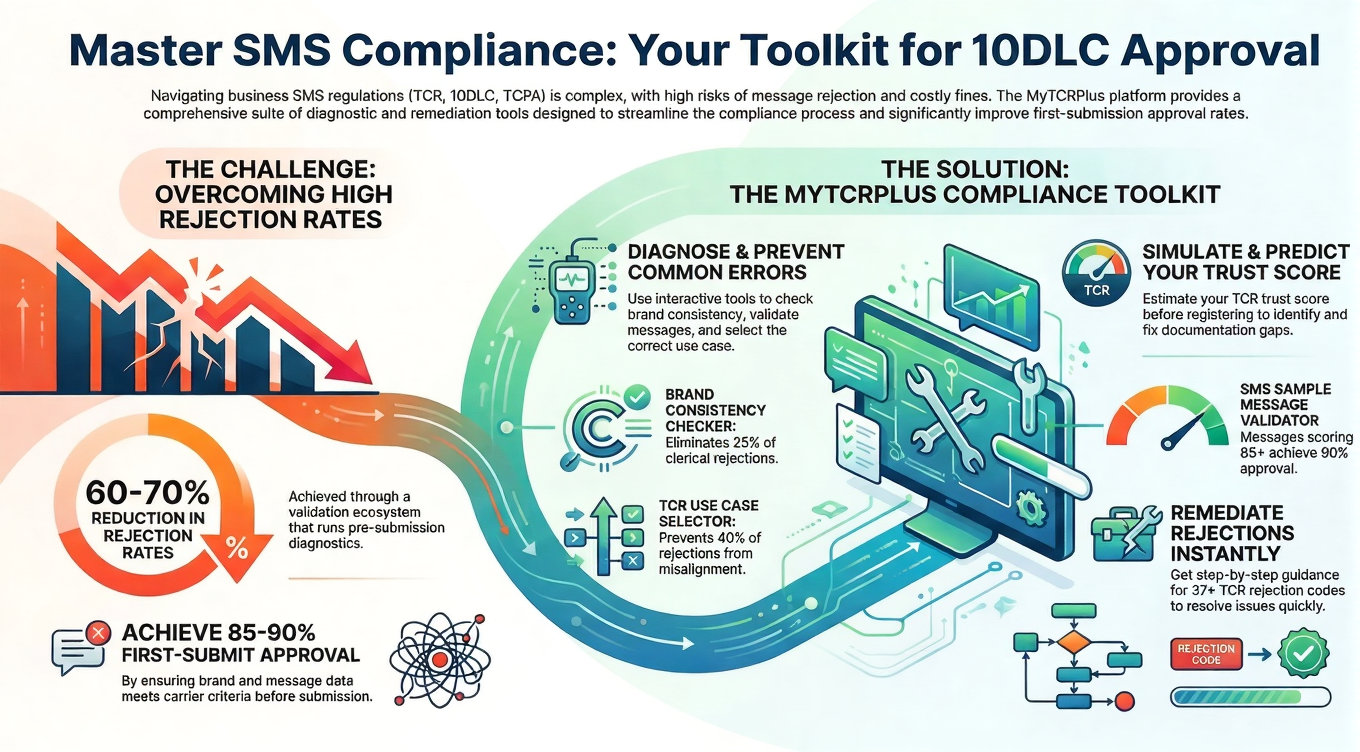
The healthcare industry stands at a critical juncture as it rapidly adopts SMS and digital messaging for patient engagement, clinical communication, and operational efficiency. This technological transformation has created a complex and nuanced compliance landscape where HIPAA privacy requirements intersect with telecommunications regulations in ways that healthcare administrators, IT directors, and compliance officers must fully understand. As healthcare providers increasingly rely on text messaging for appointment reminders, medication alerts, test results, preventive care notifications, and patient engagement initiatives, understanding the intricate relationship between HIPAA and The Campaign Registry (TCR) has become absolutely essential for maintaining both regulatory compliance and the trust that patients place in their healthcare providers.
The intersection of healthcare privacy law and telecommunications regulation represents one of the most challenging compliance environments in modern medicine. Healthcare organizations that fail to navigate this landscape properly face not only substantial financial penalties but also reputational damage that can undermine patient relationships built over years or decades. Conversely, healthcare providers that excel in this space gain a significant competitive advantage, demonstrating to patients and referring providers alike that they prioritize both privacy and communication excellence.
Understanding HIPAA: The Foundation of Healthcare Privacy Protection
HIPAA, the Health Insurance Portability and Accountability Act enacted in 1996, establishes the foundational framework for protecting patient health information in the United States. The law’s Privacy Rule, Security Rule, and Breach Notification Rule together create a comprehensive regulatory structure that applies to covered entities (healthcare providers, health plans, and healthcare clearinghouses) and their business associates.
When healthcare organizations communicate via text message or other digital channels, they must ensure that any protected health information (PHI) remains secure and that patients have explicitly consented to receive communications through these channels. Protected health information encompasses far more than many healthcare professionals realize—it includes not only obvious identifiers like medical record numbers but also combinations of data that could reasonably identify an individual, such as age combined with specific diagnoses or treatment plans.
The HIPAA Security Rule requires healthcare organizations to implement comprehensive technical safeguards to protect ePHI (electronically protected health information). These requirements include encryption of data both in transit and at rest, ensuring that messages cannot be intercepted during transmission or accessed if the device is lost or stolen. Healthcare providers must maintain detailed audit trails that document who accessed patient information, when they accessed it, and what they did with it. These audit logs become critical evidence in compliance investigations and must be retained for specified periods.
Beyond technical measures, HIPAA also requires administrative and physical safeguards. Healthcare organizations must develop comprehensive policies and procedures governing how patient information is accessed and used. They must train all workforce members on HIPAA requirements, implement access controls ensuring that each employee can access only the information necessary for their job functions, and establish clear consequences for violations.
The patient authorization requirements under HIPAA add another layer of complexity to healthcare messaging. Patients must provide specific, written authorization for certain uses of their protected health information. While routine healthcare operations like billing and treatment coordination may be conducted under the Healthcare Operations exception, using patient information for marketing communications or other secondary uses typically requires explicit patient authorization. Healthcare providers must carefully distinguish between communications that are integral to treatment or operations and those that constitute marketing, as this determination affects the authorization requirements.
The Campaign Registry: Understanding Telecommunications Compliance
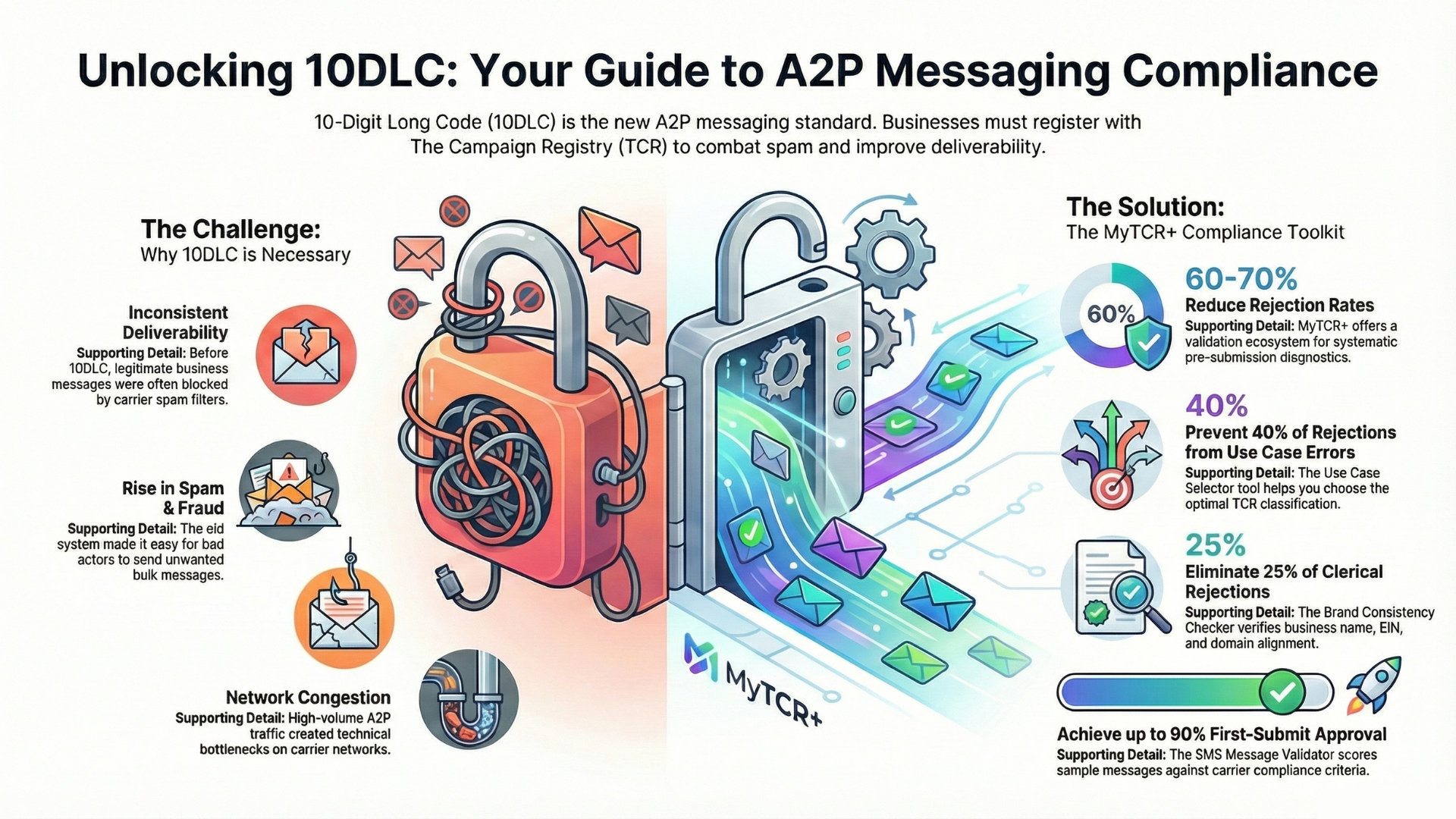
The Campaign Registry emerged as a response to the epidemic of fraudulent, spoofed, and spam text messages that have plagued American consumers in recent years. Launched by major wireless carriers including AT&T, Verizon, and T-Mobile, TCR creates a system where businesses must register their messaging campaigns and provide detailed information about their identity, the purpose of their messaging, and the recipients they intend to reach.
The registration process requires businesses to verify their legal entity information, provide evidence of legitimate business operations, and describe their specific messaging use cases in detail. Healthcare organizations must explain that they’re sending clinical communications, appointment reminders, or other healthcare-related messages. The carriers use this information to assign trust scores that directly affect message deliverability.
The concept of trust scores represents one of the most important aspects of TCR from a practical healthcare perspective. Messages from high-trust senders are more likely to bypass carrier filters and reach patient recipients reliably. Messages from low-trust or unregistered senders face increased scrutiny and are more likely to be filtered into spam folders or blocked entirely. For healthcare providers, this means that critical patient communications—appointment reminders, medication alerts, test results—may not reach patients if the TCR registration is incomplete or problematic.
TCR also establishes guidelines governing message content, frequency, and recipient consent. Carriers have developed increasingly sophisticated filters that analyze message characteristics and sender patterns, comparing them against registered use cases. Messages that deviate significantly from what was registered may be flagged or filtered. A healthcare provider that registers as sending appointment reminders but then begins sending promotional messages about new services may experience deliverability problems.
The registration process requires healthcare organizations to be transparent about their messaging practices while also maintaining patient confidentiality. This creates an interesting challenge: how can a healthcare provider describe their SMS messaging program to carriers in sufficient detail to obtain good trust scores without violating patient privacy? The answer lies in describing the types of messages and clinical purposes without including specific patient information in the registration itself.
The Intersection: Where HIPAA and TCR Requirements Converge
The true complexity of healthcare messaging compliance emerges at the intersection of HIPAA and TCR requirements. These two regulatory frameworks operate according to somewhat different philosophies and address different concerns, yet healthcare organizations must satisfy both simultaneously.
HIPAA’s primary focus is protecting patient privacy and ensuring that patients maintain control over their health information. The law emphasizes patient consent, security, and accountability. When HIPAA addresses messaging, it asks: Is the message necessary for patient care or healthcare operations? Has the patient authorized this use of their information? Is the information adequately secured? Is access properly documented and audited?
TCR’s primary focus is preventing fraud, spam, and abuse of telecommunications networks. The framework emphasizes transparency and carrier compliance. When TCR addresses healthcare messaging, it asks: Who is sending this message? What business purpose does it serve? Has the message been properly registered? Is the sender maintaining appropriate practices regarding content, frequency, and recipient consent?
These frameworks sometimes pull in different directions. HIPAA emphasizes discretion and confidentiality; TCR emphasizes transparency and disclosure. HIPAA is concerned primarily with protecting individual patients; TCR is concerned primarily with network integrity. Yet healthcare organizations cannot choose between these frameworks—they must comply with both.
One particularly nuanced challenge involves how healthcare providers describe their messaging programs in TCR registration. A complete and accurate TCR description helps ensure good deliverability for critical healthcare messages. However, healthcare providers understandably hesitate to provide detailed descriptions of their messaging practices, fearing this information could potentially compromise patient privacy or security.
The solution lies in describing messaging practices in detail while maintaining patient confidentiality. A healthcare provider can register “appointment reminders and rescheduling notifications” without describing individual patients or their appointments. They can register “medication adherence reminders and educational messages” without disclosing specific medications or patient health conditions. The goal is to help carriers understand the legitimate healthcare purpose of the messaging while respecting patient privacy.
Consent Management: The Critical Intersection Point
Consent management represents perhaps the most critical intersection between HIPAA and TCR requirements. Both frameworks require patient consent for certain communications, but they define and implement consent requirements somewhat differently.
Under HIPAA, patient consent for communications depends largely on the purpose of the message. Appointment reminders and treatment-related notifications often qualify as Healthcare Operations, which can be conducted under the general Notice of Privacy Practices without specific authorization for each communication. However, marketing communications or messages promoting healthcare services require specific written authorization. The challenge for healthcare organizations is determining which messages fall into which category.
TCR requires clear opt-in consent for text messaging enrollment. This means healthcare organizations must have documented evidence that patients explicitly agreed to receive text messages. For some communications like appointment reminders, patients might provide this consent at the time of scheduling or during patient registration. For marketing or promotional messages, the consent requirements are even more explicit.
Designing consent workflows that satisfy both HIPAA and TCR creates interesting challenges. Healthcare providers ideally should implement consent mechanisms that clearly explain how patient information will be used in messaging and specifically authorize text message delivery. The consent should distinguish between different types of messages—clinical communications, appointment reminders, billing notifications, marketing communications—so patients can make informed choices about which messages they want to receive.
Best practices involve creating modular consent frameworks where patients can authorize specific communication categories. A patient might consent to appointment reminders and medication alerts but opt out of marketing messages. This granular approach respects patient autonomy while allowing healthcare providers to maintain the communication channels necessary for efficient operations and quality care.
Healthcare organizations must document all consent decisions carefully. When a patient enrolls in text messaging, the organization should maintain records indicating when the enrollment occurred, exactly what the patient consented to, and the specific language presented to the patient. These records become critical evidence in compliance investigations and support the organization’s defense against claims that it sent unauthorized messages.
Technical Considerations: Platforms and Infrastructure
Successfully integrating HIPAA and TCR compliance requires healthcare organizations to carefully evaluate the technical platforms they use for patient messaging. Off-the-shelf consumer messaging tools like standard SMS services are inadequate because they lack the security features and audit capabilities required by HIPAA. Healthcare organizations need messaging platforms specifically designed to meet healthcare compliance requirements.
Appropriate healthcare messaging platforms should offer end-to-end encryption ensuring that messages cannot be intercepted or read during transmission. When messages travel across networks, they should be protected through industry-standard encryption protocols like TLS. Messages should also be encrypted when stored on the platform, protecting them against unauthorized access.
Comprehensive audit logging represents another essential capability. Healthcare organizations need detailed records showing which staff members accessed patient information, when they accessed it, from what location, and what actions they took. These audit logs should be tamper-proof and retained for specified periods to satisfy both HIPAA audit requirements and potential investigation or litigation needs.
TCR integration features have become increasingly important as carriers enforce registration requirements more strictly. Modern healthcare messaging platforms should include built-in features that simplify TCR registration, help healthcare organizations maintain accurate campaign descriptions, and monitor message content to ensure alignment with registered use cases. Some advanced platforms even include machine learning features that flag messages that deviate significantly from the registered use case, alerting administrators before messages are sent.
Message delivery optimization represents another important platform capability. HIPAA-compliant platforms should include sophisticated routing algorithms that maximize deliverability while respecting carrier network integrity. This includes intelligent retry logic for failed messages, delivery confirmation tracking, and integration with carrier feedback systems that help identify and resolve deliverability issues.
Two-factor authentication and granular access controls ensure that only authorized healthcare workers can access the messaging system. Employees should be able to send only messages aligned with their job functions. Supervisory and audit functions should be restricted to authorized compliance and IT personnel.
Navigating Patient Communication Through SMS and Other Digital Channels
Healthcare providers today leverage SMS for a wide variety of patient communication purposes, each with distinct compliance considerations. Appointment reminders represent the most straightforward use case. These messages serve clear operational purposes, help reduce no-shows that waste clinical resources, and generally benefit both healthcare organizations and patients. Because appointment reminders facilitate treatment, they typically qualify for HIPAA’s Healthcare Operations exception and require less extensive authorization than marketing communications.
Medication adherence reminders and alerts represent another important use case. Healthcare providers increasingly recognize that patient adherence to medications significantly impacts treatment outcomes. SMS reminders can substantially improve adherence, particularly for patients taking multiple medications or managing chronic conditions. From a compliance perspective, these messages facilitate healthcare operations and treatment, though healthcare providers should still consider whether patients prefer to receive them and maintain opt-out mechanisms.
Test result notifications and clinical alerts require particular care. When healthcare providers send messages confirming that test results are available or notifying patients of important clinical findings, these messages may contain sensitive health information. The messages must be encrypted and protected, and healthcare organizations must verify they’re sending to the correct recipient. HIPAA Breach Notification Rule requirements create significant stakes—if such a message reaches the wrong person due to an error, the healthcare organization may be obligated to notify the patient and potentially report the breach to HHS.
Preventive care and wellness communications represent a middle ground between clinical necessity and marketing. Reminders about vaccinations, health screenings, or preventive services serve legitimate healthcare purposes but may also be considered marketing in some contexts. Healthcare providers should implement clear policies distinguishing between clinical messaging (which serves core treatment or operations functions) and marketing messaging (which promotes services or products to encourage patient behavior).
Billing and insurance-related notifications serve operational purposes critical to healthcare administration. These messages might confirm payment receipt, notify patients of upcoming balance due dates, or provide insurance-related information. Because these messages facilitate necessary healthcare business operations, they typically require less extensive authorization than marketing communications.
Marketing communications promoting new services, physician practices, or healthcare programs clearly constitute marketing under HIPAA and require specific patient authorization. Healthcare organizations should not send marketing messages via SMS without documented prior express written consent, as the TCPA and CAN-SPAM Act also regulate SMS marketing in ways that HIPAA does not.
Compliance Program Development and Best Practices
Healthcare organizations serious about integrated HIPAA and TCR compliance should develop comprehensive compliance programs addressing multiple dimensions of SMS and digital messaging governance.
Policy development should establish clear standards for which message types require which types of authorization, how consent should be documented, what content is appropriate for SMS delivery, and how long messages should be retained. Policies should address incident response procedures for addressing messages sent in error or situations where messages may have reached incorrect recipients.
Staff training ensures that everyone involved in healthcare messaging understands compliance requirements. Administrative staff who schedule appointments and collect phone numbers should understand when and how they can enroll patients in SMS messaging. Clinical staff who might initiate messages should understand HIPAA requirements. IT staff should understand technical security requirements and incident response procedures.
Regular audits examine messaging practices to ensure they align with registered TCR use cases, HIPAA policies, and carrier guidelines. Audits should review sample messages to verify they don’t contain unnecessary sensitive health information, confirm that messages are sent only to consented recipients, and ensure that opt-out requests are honored promptly.
Third-party vendor management becomes critical as many healthcare organizations work with messaging service providers, IT consultants, or other vendors. Contracts with these vendors should include HIPAA-compliant business associate agreements, specify TCR compliance responsibilities, and establish audit and oversight mechanisms.
Incident response procedures should address various failure scenarios. What happens if a message is sent to an incorrect recipient? How should the organization respond to opt-out requests or unsubscribe notifications? What procedures exist for investigating message delivery failures or security incidents? Organizations should have clear procedures ensuring rapid identification, containment, and remediation of any compliance failures.
Addressing Common Compliance Challenges
Healthcare organizations frequently encounter specific challenges in integrating HIPAA and TCR compliance, and understanding how to address these challenges systematically improves overall compliance posture.
Message content challenges arise because healthcare providers want to include enough detail to ensure patients understand the message’s purpose and take appropriate action, while HIPAA encourages minimizing unnecessary transmission of sensitive health information via potentially less secure channels. The solution lies in right-sizing message content—including sufficient detail for functional purposes while avoiding unnecessary sensitive information. For example, an appointment reminder might include the appointment time, location, and provider name without including the clinical reason for the appointment if that’s not necessary for the patient to keep their appointment.
Opt-out and preference management challenges emerge as patients want different messaging options. Some patients want appointment reminders but not marketing messages. Others prefer not to receive SMS messages at all. Healthcare organizations should implement preference management systems allowing patients to control their messaging enrollments by type and update their preferences over time. These systems must be easy for patients to use, perhaps through web portals, mobile apps, or simple SMS keyword commands.
Deliverability challenges represent one of the most frustrating aspects of healthcare messaging compliance. Even properly formatted, appropriately registered messages from compliant healthcare organizations sometimes fail to reach patients due to carrier filtering or network issues. Healthcare organizations should monitor delivery rates, investigate failures, and work with messaging platforms and carriers to resolve issues. Proper TCR registration significantly improves deliverability.
Data integration challenges arise when patient contact information, consent records, and messaging history are scattered across multiple systems. Healthcare organizations should work toward integrated solutions where appointment systems, EHR systems, and messaging platforms can communicate with each other, ensuring accurate information flow and reducing error risks.
Preparing for the Future
The regulatory landscape governing healthcare messaging continues evolving as carriers update policies, regulators issue new guidance, and technology capabilities advance. Healthcare organizations must remain vigilant and adaptable.
The FCC and FTC continue enhancing enforcement of TCPA regulations and developing clearer guidance on messaging compliance. Healthcare organizations should monitor regulatory developments and adjust practices accordingly. Industry associations, healthcare legal advisors, and messaging technology providers often provide valuable updates on regulatory changes.
Carriers regularly update TCR policies, messaging guidelines, and filtering algorithms. Healthcare organizations should maintain relationships with carrier representatives, participate in industry discussions about healthcare messaging, and adjust their practices as carrier policies evolve.
Emerging technologies like artificial intelligence, advanced security measures, and new communication channels will create new compliance considerations. Healthcare organizations that establish robust compliance foundations now will be better positioned to integrate new technologies and channels while maintaining compliance.
Conclusion: Compliance as a Foundation for Trust
Successfully navigating HIPAA and TCR integration requires viewing compliance not as a burdensome obligation but as a foundation for trustworthy patient communication. Healthcare organizations that excel in this space demonstrate to patients that they prioritize both communication effectiveness and privacy protection.
When healthcare providers properly implement both HIPAA and TCR frameworks, they protect patient privacy while ensuring that important messages reliably reach the people who need them most. Appointment reminders arrive promptly, medication alerts reach patients in time to make a difference, and test results notifications inform patients of important health information without compromising security or privacy.
Healthcare organizations that invest in robust compliance programs, appropriate technology platforms, comprehensive staff training, and ongoing monitoring demonstrate their commitment to trustworthy patient communication. In an era where healthcare is increasingly competitive and patients have choices about where they receive care, demonstrating excellence in both clinical quality and communications practice creates meaningful competitive advantage while serving patients well.